Four Pillars for Rural Health Transformation

No one’s healthcare should fall through the cracks because of where they live. Yet for the 62 million people who live in rural communities across America, that’s too often their reality.
Nearly 80 percent of rural America has been designated medically underserved. Many counties lack even a single practicing physician. According to the National Rural Health Association, more than 150 rural hospitals have closed since 2010, and half of those still open are operating on negative margins.
When a hospital shutters in rural America, it is not just a building that disappears–it’s an emergency room, a maternity ward, and a hub of preventive care that vanishes from an entire community. The impact ripples across counties: patients must travel farther for basic services, towns lose jobs and economic stability, and residents grow increasingly skeptical that the healthcare system is designed to serve them at all.
For health plans and policy makers, these closures signal something deeper: miles of missing providers. More than 80 million Americans live in Health Professional Shortage Areas, where clinician gaps translate into longer wait times, delayed preventive care, and higher emergency utilization. When upstream access breaks down, downstream costs inevitably rise.
Technology has opened new doors for care delivery—but not everyone can walk through them. One in four rural adults still lack high-speed internet at home, and even where coverage exists, affordability remains a barrier. If we want telehealth to be an equalizer, it must be paired with solutions that meet patients where they are—through in-home care, device support, and community-based connectivity efforts.
Closing these gaps requires both structural investment and cultural change. CMS's Rural Health Transformation Program, which will allocate $50 billion over the next five years to strengthen rural care delivery and prevention programs, is a critical start. But funding alone won’t be enough. Transforming rural health means building lasting infrastructure for equity and sustainability. Four pillars can change the equation.
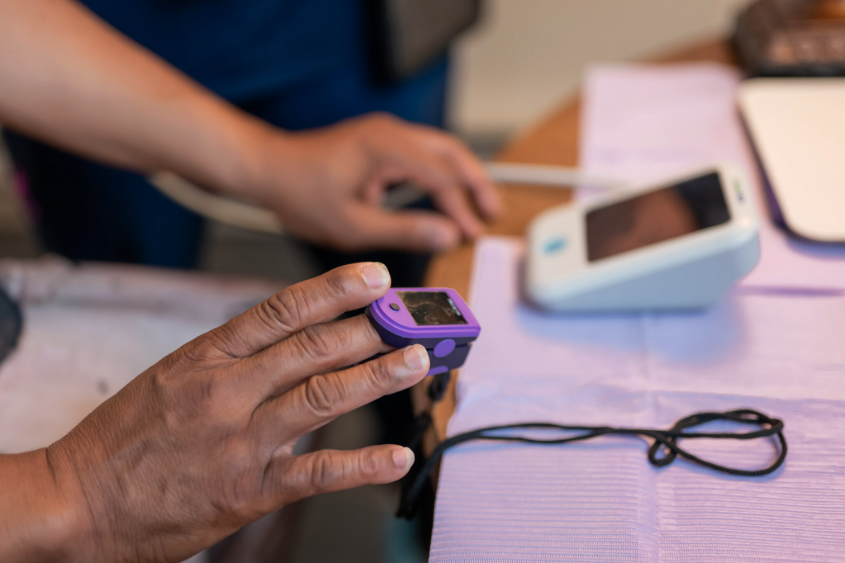
1. Meeting People Where They Are: Telehealth has expanded what’s possible—but availability doesn’t always equal access. For many patients, the leap from no care to virtual care is too far, too fast. In-home visits provide the bridge. A clinician at the kitchen table can run diagnostics, explain results in plain language, and even help set up a device for a future virtual visit. That kind of personal presence builds comfort and trust—and, over time, confidence with technology.
2. Technology That Extends Connection: AI and automation have real potential to help—not by replacing clinicians, but by freeing them to focus on patients. Smart tools can streamline documentation, optimize scheduling and routing, and flag who might need extra support. In rural regions where clinicians cover long distances, these efficiencies translate into more time spent face-to-face and less time in front of screens. Technology works best when it extends the human touch, not replaces it.
3. Strengthening the Rural Workforce: Technology and facilities mean little without the people who provide care. Many rural counties simply don’t have enough clinicians, and thin margins make recruiting and retaining them a constant challenge. Building a stable workforce requires loan-repayment programs, flexible training, and cross-training for in-home and virtual models. Most importantly, it means creating career paths that make rural practice sustainable and rewarding. No workforce, no healthcare.
4. Local Hubs for Chronic Care: Rural communities need more than one-time touchpoints—they need consistent touchpoints for managing chronic conditions like diabetes, hypertension, and heart disease. Community-based “micro-clinics” can fill this gap by combining remote monitoring with in-person follow-ups. Patients can get labs, vitals, and medication checks locally while care teams stay connected virtually for specialist input or escalation. These smaller, flexible care sites keep chronic disease management within reach and prevent hospitalizations by catching issues early.
Embedding clinicians within the communities they serve, designing care models that respect patients’ time, preferences, and lived realities, and leveraging technology in ways that extend human connection are ultimately what can make the difference.
At Sprinter Health, we’ve seen how this works in practice. Our clinicians travel into patients’ homes across diverse geographies—from rural towns to urban neighborhoods. Something as simple as noticing family photos on the wall or asking about a patient’s garden opens the door to meaningful dialogue, which is often the first step toward rebuilding trust and re-engaging people in their care.
But trust isn’t built in a single visit—it’s built at the speed of kept promises. Each follow-up, each call returned, and each reliable appointment helps patients believe the healthcare system is showing up for them. That’s especially true in rural communities, where distance, turnover, and limited connectivity have too often made healthcare feel out of reach.
The future of rural healthcare hinges on the ability of policymakers, providers, and innovators to incentivize and deliver care in ways that rural communities can recognize as theirs. Only then can we close the gaps that prevent 62 million Americans from receiving the care they need and deserve.




.png)